
An Update from Dr. Gregory Spencer
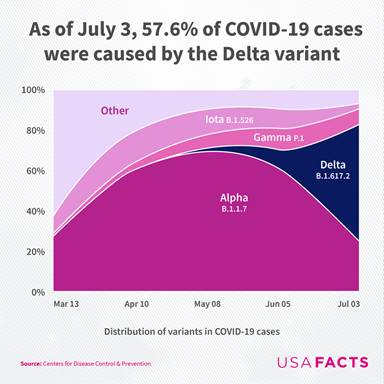
Crystal Run Healthcare has seen a spike in COVID-19 cases over the past month, similar to national trends. Reports suggest that B.1.617.2, more commonly known as the Delta variant of COVID-19, is likely driving most of the activity.
The Delta variant of COVID-19 is more infectious than the “original COVID” experienced a year ago. It also appears to have more severe symptoms and a longer transmission window. As a result, healthcare settings are reporting more “breakthrough” infections than compared to the original COVID. A breakthrough infection occurs when people who received the COVID-19 vaccine experience symptoms when infected with the Delta variant.
While effective, vaccines should be treated as the first line of defense, not an ultimate form of protection. Studies conducted last year with the original, less infectious COVID showed that COVID vaccines were 95% protective. While some people who receive the vaccine still experience symptoms after being exposed to the virus, the vaccines remain extremely effective in preventing hospitalization and death. More than 95% of the people currently hospitalized with COVID are not immunized and experience more severe symptoms than those who are vaccinated. If a vaccinated person does get infected, the vaccination tends to reduce COVID symptoms into a cold-like illness. Overall, vaccination remains the best way to avoid getting infected with COVID, being admitted to the hospital for COVID, or dying from COVID.
Some people have taken a “wait and see” approach for COVID vaccination. For those that have been hesitant, NOW is the time to get vaccinated! Why now?
The Delta variant is super infectious. In fact, it is now one of the most infectious diseases in the world. A person is much less likely to get COVID, including the Delta variant if they get vaccinated. If a vaccinated individual does get infected it will likely be mild.
- Vaccinated people will be able to do things unvaccinated people cannot do - travel, concerts, sporting events, even some weddings. Additionally, they will be less likely to spread the virus to family, friends, or coworkers.
- Hundreds of millions of people have received the COVID vaccine and it looks like these vaccines are very, very safe. It’s important to note that vaccine does not enter or alter DNA, it is considered safe for pregnant people, and there is no evidence it will affect fertility.
Some may still be hesitant to get the COVID vaccine or decide they are healthy enough to not need to get vaccinated. Statistically, most people will probably get through an acute COVID infection; however, many people report longer-lasting symptoms. More than one-third of infected people experience at least one physical symptom months after being exposed to the virus (Carfì, 2020):
- Fatigue (15 to 87 percent)
- Dyspnea (difficult or labored breathing) (10 to 71 percent)
- Chest pain or tightness (12 to 44 percent)
- Cough (17 to 34 percent)
There are also potential neurological and psychological effects (Halpin, 2020):
- Of patients with acute COVID who were discharged from the hospital:
- 24% had Post-traumatic stress disorder (PTSD)
- 18% had memory issues, with numbers being higher for those who had been in the ICU.
- In other studies, almost half of COVID survivors had worsened quality of life (Carfì, 2020):
- 22% had anxiety/ depression
- 23% had persistent psychological symptoms at 3 months.In a study of 1,300 hospitalized COVID-19 patients discharged to home, despite home health services, only 40% of patients were independent in all activities of daily living at 30 days after discharge (Bowles, 2020).
- While the persistent effects are more common for those hospitalized from COVID, even people with a mild infection may have symptoms lasting up to several months:
- A Swedish survey of over 300 health care workers showed 26% had at least one moderate or severe symptom lasting more than two months, compared with 9% of seronegative control patients (Haverall, 2021).
Crystal Run Healthcare has plenty of vaccines available. Appointments can be made online by visiting crystalrunhealthcare.com/vaccine where you can also learn more about preparing for your vaccine.
--
Gregory Spencer, MD, FACP, is the Chief Medical Officer and Chief Medical Information Officer at Crystal Run Healthcare. Dr. Spencer graduated from the Medical College of Wisconsin (Marquette University) Medical School and completed his residency in Internal Medicine while in the US Air Force at Wilford Hall USAF Medical Center in San Antonio, TX. Dr. Spencer joined Crystal Run as an internist in 1996 and was appointed as Chief Medical Officer and Chief Medical Information Officer in 2008. Dr. Spencer is board certified in Internal Medicine and is a Fellow of the American College of Physicians.
References
- Carfì A, Bernabei R, Landi F, et al. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020; 324:603.
- Xiong Q, Xu M, Li J, et al. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect 2020.
- Hopkins C, Surda P, Whitehead E, Kumar BN. Early recovery following new onset anosmia during the COVID-19 pandemic - an observational cohort study. J Otolaryngol Head Neck Surg 2020; 49:26.
- Cho RHW, To ZWH, Yeung ZWC, et al. COVID-19 Viral Load in the Severity of and Recovery From Olfactory and Gustatory Dysfunction. Laryngoscope 2020; 130:2680.
- Meini S, Suardi LR, Busoni M, et al. Olfactory and gustatory dysfunctions in 100 patients hospitalized for COVID-19: sex differences and recovery time in real-life. Eur Arch Otorhinolaryngol 2020; 277:3519.
- Halpin SJ, McIvor C, Whyatt G, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol 2020.
- Bowles KH, McDonald M, Barrón Y, et al. Surviving COVID-19 After Hospital Discharge: Symptom, Functional, and Adverse Outcomes of Home Health Recipients. Ann Intern Med 2020.
- Wong AW, Shah AS, Johnston JC, et al. Patient-reported outcome measures after COVID-19: a prospective cohort study. Eur Respir J 2020; 56.
- Nehme M, Braillard O, Alcoba G, et al. COVID-19 Symptoms: Longitudinal Evolution and Persistence in Outpatient Settings. Ann Intern Med 2020.
- Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2020.
- Logue J K; Franko N M; McCulloch D J; et al. Sequelae in Adults at 6 Months After COVID-19 Infection JAMA Network Open. 2021;4(2):e210830.
- Mandal S, Barnett J, Brill S, et al. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2020; PMID 33172844.
- Bellan M, Soddu D, Balbo PE, et al. Respiratory and Psychophysical Sequelae Among Patients With COVID-19 Four Months After Hospital Discharge. JAMA Netw Open. 2021;4(1):e2036142.
- Writing Committee for the COMEBAC Study Group, Morin L, Savale L, Pham T, et al. Four-Month Clinical Status of a Cohort of Patients After Hospitalization for COVID-19. JAMA. 2021; PMID 33729425.
- Del Brutto OH, Wu S, Mera A, Recalde et al. Cognitive decline among individuals with history of mild symptomatic SARS‐CoV‐2 infection: A longitudinal prospective study nested to a population cohort. Eur J Neurol 2021; PMID 33576150.

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Same and next-day pediatric appointments
Same and next-day pediatric appointments