Vein Center
Welcome to the Vein Center at Crystal Run Healthcare. Our skilled vascular physicians treat the full spectrum of conditions affecting the veins, including varicose veins, spider veins, and deep vein thrombosis (DVT).
Our physicians use minimally-invasive surgical techniques whenever possible and the most advanced equipment available to ensure less pain and faster recovery times.
Most of the procedures we offer are performed on an outpatient basis, meaning they do not require a hospital stay or sedation under general anesthesia. This means you can resume your normal activities more quickly—in some cases immediately after surgery.
Conditions We Treat
Varicose and Spider Veins
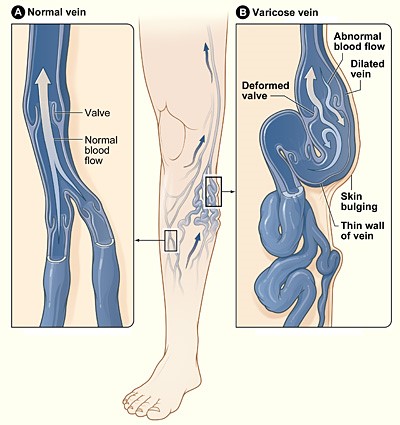
Varicose veins are gnarled, enlarged veins, often with a cord-like appearance. They develop when the valves that direct blood flow through the veins don’t work as they should.
Varicose veins can develop anywhere in the body, but they most often affect the legs and feet because standing and walking increase the pressure on the veins in the lower part of the body.
Spider veins are a more mild variation of varicose veins. They appear as thin, wispy veins on the surface of the skin. Unlike varicose veins, which sometimes cause pain or discomfort, spider veins are generally only a cosmetic problem.
Causes and risk factors for varicose and spider veins can include:
- Standing for hours on the job
- Obesity
- Using birth control pills or hormone replacement therapy (HRT)
- Having a history of blood clots
- Hormonal changes that occur during pregnancy, puberty, and menopause
- Chronic constipation
- Constriction of the abdomen (e.g., from wearing constrictive clothing)
Symptoms of Varicose and Spider Veins
Many people with varicose veins experience painful aching or cramping in the legs. Other symptoms can include throbbing, fatigue, or a feeling of heaviness in the legs. Some people also experience burning or tingling sensations or itching around one or more veins. Bleeding from one or more varicose veins can also occur.
Elevating the legs and wearing graduated support stockings can help relieve symptoms.
Complications of Varicose Veins
In more severe cases, veins may harden or change colors. These changes, along with skin ulcers near the ankles, can indicate a more serious form of vascular disease.
Some people with varicose veins will develop blood clots near the surface of the skin that cause inflammation and swelling (thrombophlebitis). This can lead to a more serious condition called deep vein thrombosis (DVT), a condition that causes blood clots to form in the deep veins of the legs; a DVT blood clot can break off and move to the lungs, leading to pulmonary embolism, a life-threatening condition.
Treatment for Varicose and Spider Veins
Conservative treatments for varicose veins include lifestyle changes: wearing support stockings, managing your weight, practicing good hygiene, and walking regularly. Your doctor may also recommend one or more of following treatments:
- Sclerotherapy: Involves injecting a highly-concentrated saline solution into the vein(s), causing the vein to gradually disappear over a period of three to six weeks. Sclerotherapy can be performed in an outpatient (non-hospital) setting. For larger veins, your doctor may use a newer technique called foam sclerotherapy, where a foam solution is injected into the vein to close and seal it.
- Endovenous laser treatment (VeneCure™): Uses small pulses of laser light to collapse varicose veins; the procedure is typically performed on an outpatient basis under local, non-sedating anesthesia.
- Phlebectomy: A minimally invasive procedure in which small veins near the surface of the skin are removed through small punctures; a phlebectomy is done on an outpatient basis using local anesthesia called Lidocaine.
- Radiofrequency occlusion (Venefit™): Uses radiofrequency energy delivered via a catheter to heat, collapse, and seal the varicose vein shut; radiofrequency occlusion is typically performed on an outpatient basis under local anesthesia.
- Vein stripping and ligation: This procedure involves tying off a vein and removing it through small incisions. To prevent blood circulation problems in the leg, the vein is removed before the section where it meets a deep vein. Stripping and ligation is a surgical procedure typically performed in a hospital setting under general anesthesia; because it is more invasive, ligation and stripping are used less frequently today, but may be necessary for patients with more severe vein problems e.g., venous insufficiency or valvular regurgitation.
VNUS Closure™: The VNUS Closure™ procedure is a minimally invasive varicose vein surgery for people suffering from superficial venous reflux, the major underlying cause of painful, swollen, disfiguring veins (varicose veins). The Closure system provides an alternative to painful vein stripping surgery or laser vein ablation with a disposable radiofrequency catheter that controllably heats and closes diseased veins in a procedure that can take 30 minutes or less.
Deep Vein Thrombosis & Pulmonary Embolism
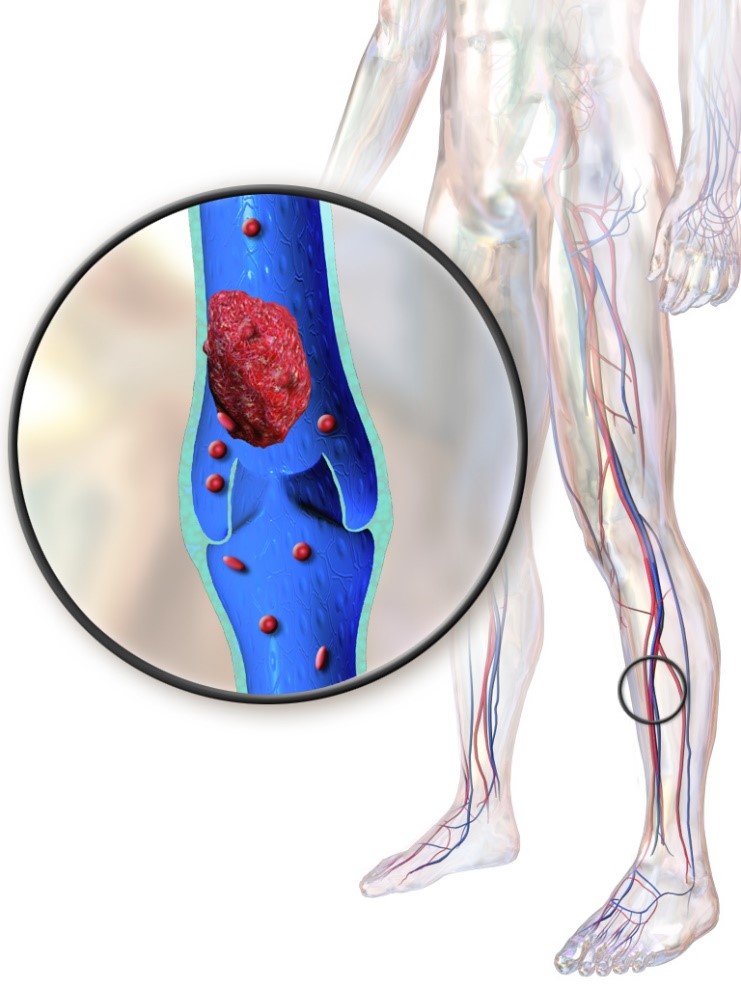
Deep vein thrombosis (DVT) is when a blood clot forms in a deep vein, usually in the leg. Inherited blood-clotting disorders, prolonged bed rest, and injury to a vein during surgery are all possible causes of DVT. Heart failure, smoking, and cancer can also lead to DVT blood clots.
Symptoms of DVT and Pulmonary Embolism
Symptoms of deep vein thrombosis can include leg pain and swelling, red or discolored skin on the leg, and a feeling of warmth on the leg. However, some people may have no noticeable symptoms.
A DVT blood clot can lead to a life-threatening condition called pulmonary embolism, which is when the clot breaks off and travels to the lung, blocking an artery. Symptoms of pulmonary embolism include chest pain or discomfort, sudden shortness of breath, lightheadedness or dizziness, rapid pulse, and coughing up blood.
Treatment for DVT and Pulmonary Embolism
In some cases, conservative treatments may be enough. These include blood thinners and clot-busting medications, as well as compression stockings.
In more severe cases, your doctor may recommend the following treatments:
- Vena cava filter placement: People who can’t take blood thinning medications may need to have a filter placed inside the vena cava, a large vein in the abdomen; the filter prevents clots from traveling to the lungs.
- Venous thrombolysis: This procedure is suitable for people with acute DVT; the doctor uses a small catheter to access the blood clot and then injects a medication to slowly dissolve the clot.
- EKOS® procedure: This procedure delivers clot-busting medicine directly to the clot and uses ultrasound energy to loosen the clot and allow the medication to work more effectively.
- Pulmonary embolism surgery: In rare cases, a person may need surgery to remove a blood clot from the lung.
Vascular Thoracic Outlet Syndrome
Thoracic outlet syndrome is a group of disorders that occur when the blood vessels that supply blood to the arm become compressed. Vascular thoracic outlet syndrome is when one or more of the veins or arteries under the collarbone becomes compressed.
It can happen from physical trauma (such as a car accident), from an anatomical defect (such as having an extra rib), or even pregnancy.
Symptoms of Vascular Thoracic Outlet Syndrome
Signs and symptoms of vascular thoracic outlet syndrome can include:
- Cold fingers, hands, or arms
- Numbness or tingling in arms, hands, or fingers
- Arm pain and swelling
- Discoloration or lack of color in fingers, hands, or arms
- Arm fatigue with activity
- General arm weakness
- Weak or no pulse in affected arm
- Blood clot in veins or arteries of upper body
Diagnosis and Treatment for Vascular Thoracic Outlet Syndrome
Some of the signs and symptoms of vascular thoracic outlet syndrome are similar to those of other conditions, including certain diseases of the cervical spine (neck). To make an accurate diagnosis, your doctor may order any of the following tests:
- X-ray
- Ultrasound
- Computed tomography angiography (CTA)
- Magnetic resonance imaging (MRI)
- Nerve conduction study (identifies nerve damage)
- Electromyography (records electrical activity of muscle tissue)
- Arteriography & venography (produces images of arteries and veins using a dye and X-rays)
Treatments can include:
- Physical therapy
- Anti-inflammatory medications
- Clot-dissolving medications (thrombolytic therapy)
- Surgery (thoracic outlet decompression; there are several surgical approaches, including the infraclavicular approach, in which the surgeon makes an incision under the collarbone to repair compressed veins)
Experts in Treating Vascular Diseases and Conditions
The skilled physicians at Crystal Run Healthcare expertly diagnose and treat the full spectrum of vascular diseases, including varicose and spider veins, chronic venous insufficiency, deep vein thrombosis, vascular thoracic outlet syndrome, peripheral artery disease, May-Thurner syndrome, Paget-Schroetter syndrome, and others.
We listen carefully to your needs and concerns and work closely with you to develop a comprehensive treatment plan and the long-term lifestyle changes that are often needed to help keep your vascular system healthy. These lifestyle changes can include adopting a healthy diet, exercising regularly, taking all prescribed medications as directed, and managing your weight.
We also work closely with other Crystal Run Healthcare specialists as needed to provide you with a complete continuum of care. Schedule an appointment with one of our vein specialists today.

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Same and next-day pediatric appointments
Same and next-day pediatric appointments